What is Endometriosis?
Endometriosis is a chronic inflammatory condition that significantly impacts the quality of life of millions of women worldwide. It is characterized by the presence of endometrial-like tissue outside the uterus, most commonly on the ovaries, fallopian tubes, and pelvic peritoneum. These ectopic cells respond to hormonal fluctuations, particularly estrogen, leading to cyclical growth, inflammation, and the formation of lesions, adhesions, and scar tissue. Over time, this can contribute to debilitating pelvic pain, painful menstruation (dysmenorrhea), pain during intercourse (dyspareunia), and even fertility challenges. Endometriosis is also associated with immune system dysregulation, increased oxidative stress, and altered gut microbiota, further exacerbating inflammation and symptoms. Despite its prevalence, the condition is often underdiagnosed and can take years to be properly identified, highlighting the need for greater awareness, research, and integrative treatment approaches.
Symptoms can vary widely and may include:
- pelvic pain
- bloating
- heavy or irregular periods
- abdominal discomfort
- fatigue/low energy
- fertility complications
- pain during or after sex
- diarrhoea or constipation during a menstrual period
- pain with urination
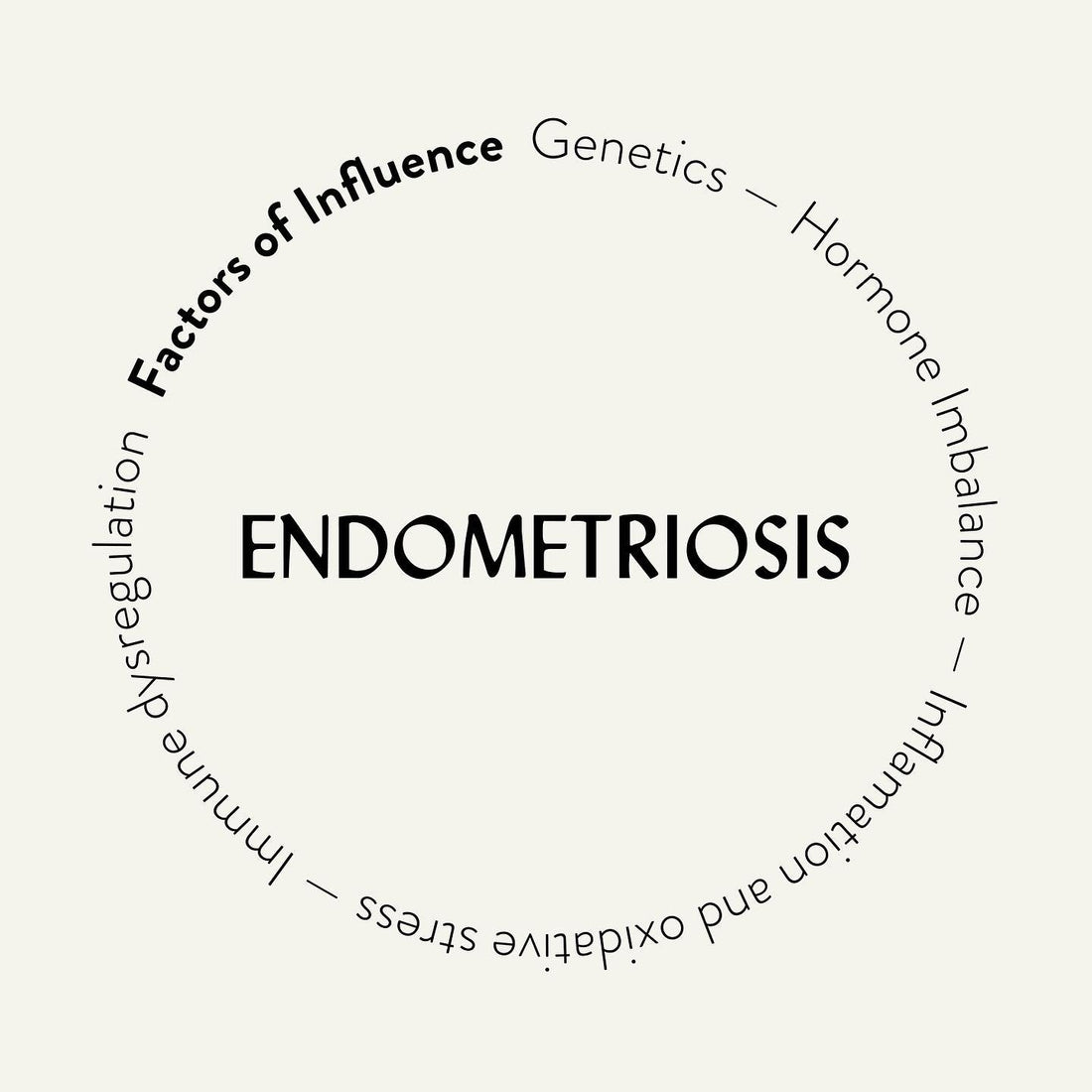
What drives endometriosis?
Endometriosis root cause remains misunderstood, however there are a few theories as to what may drive endometriosis
Hormone Imbalances
Endometriosis is considered an estrogen-dependent condition, meaning that elevated estrogen levels or increased estrogen sensitivity can contribute to the growth and inflammation of endometrial-like tissue. Potential hormonal imbalances that may drive endometriosis include:
- Estrogen dominance, where estrogen levels are too high relative to progesterone, leading to increased tissue growth and inflammation.
- Progesterone resistance, where the body does not respond effectively to progesterone, which is essential for balancing estrogen’s effects.
- Cortisol dysregulation, where chronic stress affects adrenal function, leading to further hormone imbalances and inflammation.
Gut Microbiome Imbalances
The gut microbiome plays a crucial role in immune function, hormone metabolism, and inflammation—three key factors linked to endometriosis. Research suggests that individuals with endometriosis often have an altered gut microbiome, with higher levels of inflammatory bacteria and lower levels of beneficial microbes. This imbalance may contribute to:
- Increased intestinal permeability (leaky gut), allowing toxins and inflammatory compounds to enter the bloodstream.
- Higher estrogen reabsorption, as gut bacteria help regulate estrogen levels through the estrobolome (a subset of the microbiome involved in estrogen metabolism).
- Chronic inflammation, which is a major driver of endometriosis symptoms and progression.
Genetics
There is a hereditary component to endometriosis, meaning if a close relative (such as a mother or sister) has the condition, the likelihood of developing it increases. Genetic research has identified specific gene mutations and variations that may contribute to:
- Altered inflammatory responses, making some individuals more susceptible to chronic inflammation.
- Changes in hormone sensitivity, leading to an increased response to estrogen, which fuels endometrial tissue growth.
- Differences in immune system function, which may allow endometrial tissue to implant and grow outside the uterus.
Immune Dysregulation
The immune system plays a role in identifying and clearing misplaced endometrial tissue. In those with endometriosis, immune dysfunction may contribute to:
- Reduced ability to remove ectopic endometrial cells, allowing them to implant and grow.
- Chronic inflammation, which worsens pain and promotes disease progression.
- Increased autoimmunity, as some research suggests endometriosis may have autoimmune-like characteristics, with higher levels of inflammatory markers and immune dysfunction.
While the exact cause of endometriosis remains unknown, these factors likely interact in complex ways, making a holistic approach—including gut health, hormone balance, and immune support—key in managing symptoms naturally.